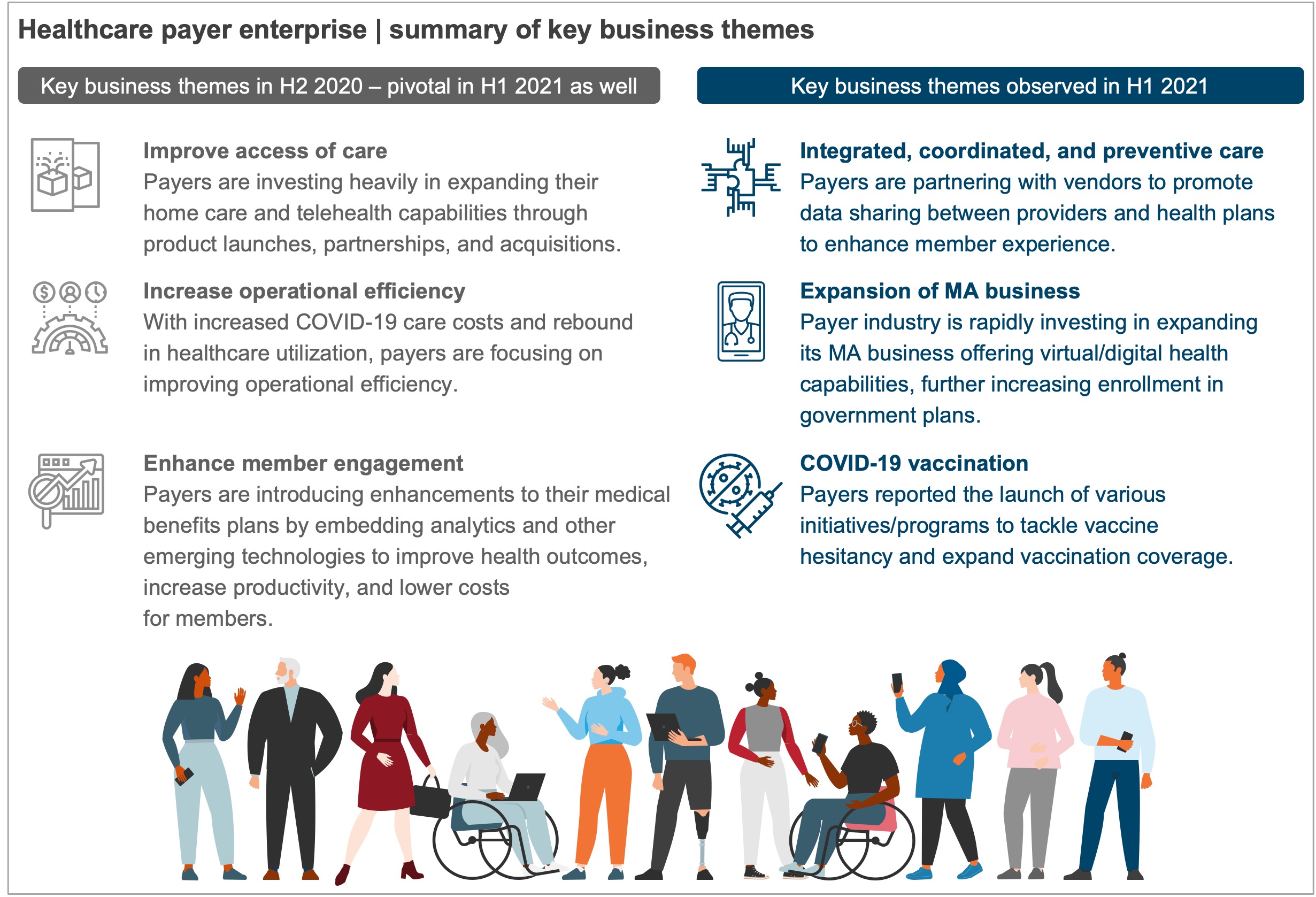
COVID-19 has fundamentally altered the functioning of the healthcare industry by significantly changing who receives care and how they access it. The pandemic has also posed several challenges for payers, such as disruption of member service operations, administrative inefficiencies around provider network management/coordination, member communication, and claims management. Now that the dust is settling and organizations are again turning profitable, they are looking beyond the immediate issues of cost takeout, care delivery, and capacity utilization toward building resilient business models, improving care outcomes, and enhancing the experience of healthcare users, including physicians, patients, and members.
In fact, payers reported substantial profits in Q1 2021. Higher enrollment in government plans drove growth, especially for Medicare Advantage (MA) plans, though commercial enrollment was still below pre-pandemic levels. Healthcare enterprises are realizing the need to build coordinated, integrated, and preventive care as they shift to value-based care and look to bring down costs while improving the quality of care. Payers are increasingly developing strategies to build new home-based health models, strengthen population health initiatives, and facilitate better coordination between different forms of care.
This report examines payer performance in H1 2021. It focuses on industry- and account-level financial and Line of Business (LoB) performance. and key business and IT investment themes.
Scope
The report examines payer performance at an industry and account level.
Industry: healthcare payer
Geography: US
Contents
In this research, we:
- Provide a payer industry overview: financials, membership by LoB, business themes, and IT themes
- Share account-specific insights: financials, membership by LoB, and account-specific themes
Membership(s)
Healthcare Payer and Provider Information Technology
Sourcing and Vendor Management